Iwatsuki, M., Takada, S., Mori, M. et al. In vitro and in vivo antimalarial activity of puberulic acid and its new analogs, viticolins A–C, produced by Penicillium sp. FKI-4410. J Antibiot 64, 183–188 (2011). https://doi.org/10.1038/ja.2010.124
概要
抗マラリア薬のスクリーニングの過程で、Penicillium sp. FKI-4410の培養ブロスから5種類のトロポロン化合物が単離された。 そのうち2つは既知の化合物であるpuberulic acidとstipitatic acidであった。 そのうち3種はプベルル酸の新しい類縁体であり、viticolins A-Cと命名された。 このうち、プベルル酸はin vitroでクロロキン感受性および耐性マラリア原虫株に対して0.01 μg ml-1のIC50値を示し、強力な抗マラリア阻害作用を示した。 さらに、プベルル酸はヒトMRC-5細胞に対して弱い細胞毒性を示し、IC50値は57.2μg ml-1であった。 また、この化合物はin vivoで治療効果を示し、現在使用されている抗マラリア薬と比較して良好であったことから、新規抗マラリア化合物への開発の有力候補として期待される。
試験管内での抗マラリア活性
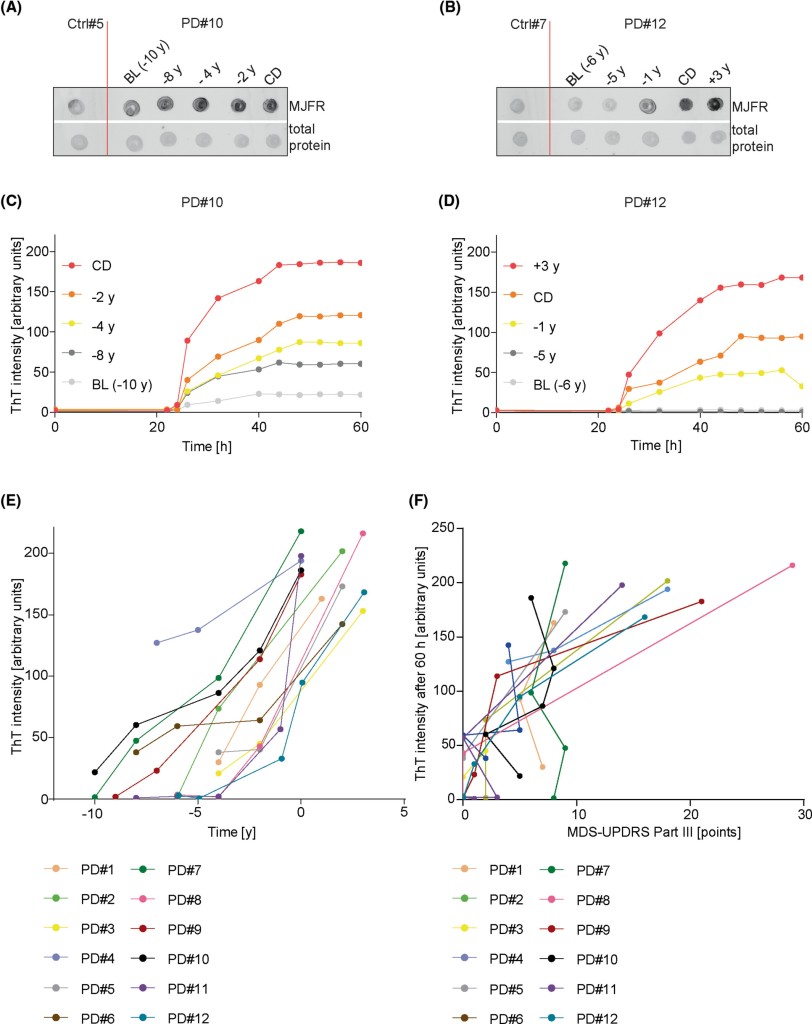
表3は、単離された化合物のin vitro抗マラリア活性を、他の既知のトロポン化合物およびいくつかの標準抗マラリア薬とともに示したものである。 プベルリン酸(1)は、P. falciparumのクロロキン耐性K1株およびクロロキン感受性FCR3株の両方に対して、顕著な強力かつ均一な活性を示した。 K1株とFCR3株に対する抗マラリア活性は同一であった(0.01 μg ml-1)。 K1株に対する1の活性は、アルテミシニンまたはアルテスネートと同程度であった。 試験した他のすべての化合物の抗マラリア性は比較的弱かった。 K1株に対して、ビチコリンB(4)と7-ヒドロキシトロポロンはそれぞれ0.84と0.89μg ml-1のIC50値を示した。 Viticolin A (3)、stipitatic acid (2)、troponeとhinokitiolはさらに弱い抗マラリア活性を示し、5-10μg ml-1の範囲であった。 ビチコリンC(5)とトロポロンは抗マラリア活性を示さなかった。
試験したトロポロンのうち、ヒノキチオールとトロポロンのFCB株NC-1に対するIC50値は、それぞれ0.5と3.7μg ml-1であった。 この2つの結果の違いは、アッセイ条件の違いか、使用したPlasmodium株の違いによると考えられる。
試験化合物の細胞毒性を表3に示す。 単離された化合物およびトロポンは,7-ヒドロキシトロポロン(IC50=0.24 μg ml-1)を除いて,弱い細胞毒性(IC50=5〜60 μg ml-1)または細胞毒性を示さなかった。 抗マラリア活性と細胞毒性を合わせて評価するために、表3に示すように、選択性指標(細胞毒性(MRC-5細胞に対するIC50)/抗マラリア活性(K1株またはFCR-3株に対するIC50))を導入した。 プベルル酸(1)は、寄生虫の系統に関係なく5720という比較的高い選択性を示し、クロロキンの選択性を大きく上回った。 試験した他のすべての化合物のうち、良好な選択性指数を示したものはなかった。
生体内抗マラリア活性
クロロキン感受性のげっ歯類マラリアP. berghei N株を用いて、プベルル酸および標準的な抗マラリア薬のin vivo抗マラリア活性をマウスモデルで予備的に測定した。 1 2 mg kg-1の投与により、マラリア原虫の69%が抑制された。 同じ実験条件下で、アルテスネートおよびクロロキンのED50値は、それぞれ1.7および1.5 mg kg-1であった。プベルル酸のin vivo s.c.抗マラリア活性がアルテスネートおよびクロロキンの両方に類似しているという最初の発見は、プベルル酸がリード抗マラリア化合物として実質的に有望であることを確認するものである。
考察
我々はプベルル酸(1)、スティピタット酸(2)および構造的に関連する新規化合物であるビチコリンA-C(3-5)を単離した。 これら5つの化合物のin vitroでの抗マラリアおよび細胞毒性研究は、他の既知のトロポン化合物とともに、構造活性相関に関する貴重な洞察をもたらした。
プベルル酸のC-7にあるヒドロキシ基は抗マラリア活性にとって重要な部位であると思われる。 C-7にメトキシ基を持つ化合物3と4、およびC-7にヒドロキシ基を持たない化合物2は、それぞれ1の1,000倍、80倍、700倍活性が低かった。 さらに、C-7にヒドロキシ基を持つ7-ヒドロキシトロポロンはトロポロンより14倍活性が高かった。 プベルル酸のC-4のカルボキシル基は選択性に関して重要であると思われる。 C-4にカルボキシル基を持つ化合物1と2は、7-ヒドロキシトロポンとヒノキチオールよりも優れた選択性指数を示した。 3のC-2のメトキシ基も抗マラリア活性を向上させるようである。 このことは、1の2-O-メチル類似体が1よりも強力な抗マラリア活性を持つことを示しているのかもしれない。1およびその類似体の詳細な構造と活性の関係をより包括的に理解するためには、さらなる研究が必要である。
一般に、天然および合成のトロポロン類は、抗菌、抗真菌、殺虫、抗ウイルス、抗腫瘍活性を示し、アミノグリコシド-2″-O-アデニル転移酵素17、メタロプロテアーゼ18、HIV-1逆転写酵素関連リボヌクレアーゼHなどの酵素を阻害することが報告されている19。 これらの化合物のうち、ヒノキチオールとその関連合成誘導体が抗マラリア活性を示すことが報告されており、合成ベンゾトロポロン誘導体15, 21, 22とジヒドロトロポロン抗生物質であるコルジトロポロン23もin vitroで中程度または弱い抗マラリア活性を示すことが報告されている。 しかしながら、本論文はプベルリン酸のようなカルボキシトロポロン類の抗マラリア活性に関する最初の報告である。
以上の結果から、プベルル酸は新規抗マラリア薬開発のための有望なリード化合物であることが示された。 プベルル酸の抗マラリア能については、広範なin vivo試験を含むさらなる研究が進行中である。
→in vivo 試験が進行中であると、考察の最後に述べているが、このin vivo試験の論文を見つけることはできなかった。
Antimalarial tropones and their Plasmodium falciparum glyoxalase I (pfGLOI) inhibitory activity
Aki Ishiyama, Masato Iwatsuki, Tsuyoshi Yamamoto, Hiromi Miura, Satoshi Ōmura, Kazuhiko Otoguro
The Journal of Antibiotics 67 (7), 545-547, 2014
https://doi.org/10.1038/ja.2014.28
→in vivo試験の記載なし。
Sennari, G., Saito, R., Hirose, T. et al. Antimalarial troponoids, puberulic acid and viticolins; divergent synthesis and structure-activity relationship studies. Sci Rep 7, 7259 (2017). https://doi.org/10.1038/s41598-017-07718-3
要旨
天然に存在する化合物を含む抗マラリア性トロポノイドの多様な合成が、プベルル酸の全合成経路を利用して達成された。 天然物と単純なトロポノイドの構造活性相関から、我々はこのクラスの化合物のより詳細な特性を探求することになった。 プベルル酸の全合成において、7-ヒドロキシトロポロン類を提供するための段階的な酸化-芳香族化と、カルボン酸部分の変換のための臭素化のシーケンスにより生成した中間体化合物を通して、新規誘導体へのアクセスが容易になった。 ビチコリンAの最初の全合成、および異なるメチル置換誘導体の合成も達成した。 新規誘導体のin vitro抗マラリア活性および細胞毒性を評価し、より有望な抗マラリア薬の探索を促進するための基礎情報を得た。
はじめに
世界で最も深刻な感染症のひとつであるマラリアは、特にサハラ以南のアフリカにおいて、依然として深刻な世界的健康問題となっている。 世界保健機関(WHO)は、2015年のマラリアの臨床患者数は2億1200万人、死亡者数は42万9000人と推定し、世界人口の約半分にあたる32億人を危険にさらしていると警告している1。 マラリア治療薬としてキニーネ2、クロロキン3、スルファドキシン/ピリメタミン4など様々な伝統的な抗マラリア薬が開発され、さらに現在のアルテミシニンベースの併用療法(ACT)5があるにもかかわらず、薬剤耐性寄生虫やACTに対する多剤耐性が急速に、かつ継続的に出現している6。 そのため、新しい構造と新しい作用機序を持つ抗マラリア薬の開発が、絶え間なく緊急に求められている。
Penicillium viticola 9 FKI-4410の培養ブロスから、新規天然物であるプベルル酸(1)7、スティピタット酸(2)8、ビチコリンAおよびB(3, 4)が我々のスクリーニング系により単離され、有望な抗マラリア活性を有することが見出された(図1)10, 11。 これらの高酸素性7員環芳香族化合物の中で、1はマラリア原虫K1株(クロロキン耐性)に対してin vitroで最も強力な抗マラリア活性を示し(IC50 = 0.050 µM)、またin vivoでは、P. berghei感染モデルマウスを用いた4日間の抑制試験において、皮下(s.c.)投与による2 mg/kg × 4の用量で69%の阻害効果を示した12。 しかし、1(プベルル酸)はin vivoで毒性を示し、5 mg/kg×2(0日目と1日目)のs.c.投与後、3日目までに5匹中4匹のマウスが死亡した。 トロポン(5)、トロポロン(6)、ヒノキチオール(8)などの構造的に単純な化合物や、天然の2および3は、1の活性よりも弱い活性を示したが、7-ヒドロキシトロポロン(7)13ははるかに強力で、5のそれよりも18倍以上強いIC50値6.44μMを示した。 この観察から、化合物中に連続する酸素原子が 3 つ以上存在することが、抗マラリア活性に大きく影響する可能性が示唆された。 この結果を契機に、全合成ルートの確立に基づく構造活性相関(SAR)研究を実施し、強力な抗マラリア活性を保持し、かつ無毒性の新規抗マラリア候補化合物の創製を目指した。 さらに、これらの化合物の特性、特に低分子量と単純な平面構造は、効率的かつ実用的な合成によって可能になる供給の容易さ14の点で、抗マラリア薬のリード化合物として貴重なものになると期待された。 ここでは、確立された1 15の全合成経路を利用して、天然物を含むいくつかの関連トロポノイドを分岐合成し、in vitroでの抗マラリア活性と細胞毒性を生物学的に評価した結果を報告する。
→序論で、マウスに皮下投与した場合の高い致死率を記載しているが、引用文献には、そうような記載のある論文はなし。
7. Birkinshaw, J. H. & Raistrick, H. Studies in the biochemistry of micro-organisms, XXIII. Puberulic acid C8H6O6 and an acid C8H4O6, new products of the metabolism of glucose by Penicllium puberulum Bainler and Penicillium aurantio-virens Biourge. With an appendix on certain dihydroxybenzenecarboxylic acids. Biochem. J. 26, 441–453 (1932).
8. Birkinshaw, J. H., Chambers, A. R. & Raistrich, H. Studies in the biochemistry of micro-organisms. Stipitatic acid, C8H6O5, a metabolic product of Penicillium stipitatum Thom. Biochem. J. 36, 242–251 (1942)
9. Nonaka, K. et al. Penicillium viticola, a new species isolated from a grape in Japan. Mycoscience 52, 338–343 (2011)
10.Iwatsuki, M. et al. In vitro and in vivo antimalarial activity of puberulic acid and its new analogs, viticolins A–C, produced by Penicillium sp. FKI-4410. J. Antibiot. 64, 183–188 (2011).
11. Ishiyama, A. et al. Antimalarial tropones and their Plasmodium falciparum glyoxalase I (pfGLOI) inhibitory activity. J. Antibiot. 67, 545–547 (2014)
12. Peters, W., Portus, J. H. & Robinson, B. L. The chemotherapy of rodent malaria, XXII. The value of drug-resistant strains of P. berghei in screening for blood schizonticidal activity. Ann. Trop. Med. Parasitol. 69, 155–171 (1975).
学位論文 博士論文 2021(令和3)年度 甲
Puberulic acidの誘導体合成およびAvermectin類の収束的合成法の確立
感染制御科学専攻 創薬科学履修コース 生物有機化学 DI-19002 齋藤 亮 「抗マラリア薬創製を指向したPuberulic acid類の合成と構造活性相関研究」
【目的】 世界三大感染症の一つであるマラリアは、既存薬に耐性を持つ原虫の増加により新規作用機序を持つ治療薬の開発が急務である1)。また、蔓延地域の衛生的・経済的状況から、新薬には経口薬として効果を示すことが求められる。この背景の下、所属研究所においてpuberulic acid (1)(Fig. 1)が新規糸状菌から単離された2)。その構造的特徴として、高度に酸素官能基化された非ベンゼン系7員環芳香族であるトロポロン骨格を持つ。1は薬剤耐性原虫を用いたin vitro抗マラリア活性試験で高活性を示し、新規作用機序を持つと期待される3)。しかし、1はネズミマラリア感染マウスを用いたin vivo試験では皮下投与で毒性を示し、経口投与では治療効果を示さなかった。そこで新規抗マラリア薬の開発を目的に1の誘導化による構造活性相関の解明と、経口投与に有効で且つ無毒性な化合物の創製を目指した。
→プベルル酸のin vivo試験での毒性を記載しているが、それを論じた引用文献なし。
https://acrobat.adobe.com/id/urn:aaid:sc:AP:6bda7cb9-8787-47b4-bea8-508e87290065
Discoveries and Syntheses of Highly Potent Antimalarial Troponoids
Ryo Saito, Goh Sennari, Asuka Nakajima, Aoi Kimishima, Masato Iwatsuki, Aki Ishiyama, Rei Hokari, Tomoyasu Hirose, Toshiaki Sunazuka
キーワード: puberulic acid, viticolin, tropolone, tropone, structure–activity relationship, natural product
Chemical and Pharmaceutical Bulletin
2021 年 69 巻 6 号 p. 564-572
https://www.jstage.jst.go.jp/article/cpb/69/6/69_c21-00132/_html/-char/ja
要旨
プベルル酸の新規誘導体を合成し、Plasmodium falciparum K1株に対するin vitroでの抗マラリア作用、ヒト二倍体胚細胞株MRC-5に対する細胞毒性、およびPlasmodium berghei感染マウスモデルを用いたin vivoでの有効性を評価した。 トロポン骨格上の3つのヒドロキシ基が抗マラリア活性に必須であるという以前の情報から、我々はカルボン酸部分を対応するエステル、アミド、ケトンに変換した。 これらの誘導体は、in vitroでクロロキン耐性原虫に対してプベルル酸と同等の抗マラリア活性を示した。 我々は、ペンタン-3-イルエステル、シクロヘキシルエステル、iso-ブチルケトン、シクロヘキシルメチルケトンが、いずれも15 mg/kgの経口投与で、明らかな毒性を示すことなく、生体内で特に強力な抗寄生虫効果を示すことを確認した。 これらのエステルは、一般的に使用されている既存の抗マラリア薬であるアルテスネートよりも有効であった。
はじめに
マラリアは、感染したアノフェレス蚊に刺されることで人に感染する寄生虫によって引き起こされる、生命を脅かす病気である。 WHO1)によると、2019年には87のマラリア流行国で2億2900万人のマラリア患者が発生し、409000人の命が奪われた。 WHOはマラリア対策として、作用機序の異なる2種類以上の薬剤を使用する併用療法を推奨しており、主にアルテミシニンをベースとした併用療法(ACT)が用いられている2)。 サハラ以南のアフリカでは、保健システムが比較的不十分で、人員や資源が不足しており、貧困の状況が続いているため、薬剤耐性寄生虫が急速に進化することが知られている1)。 マラリアは、感染したアノフェレス蚊に刺されることによって人に感染し、生命を脅かす病気である。そのため、新しい作用機序を有し、適切な価格で入手でき、脆弱な人々にも容易かつ安全に使用できる治療薬が、緊急かつ強く求められている。 また、そのような状況では非経口薬よりも経口薬の方が投与の面で望ましい3)。
我々は、スクリーニングプログラム、化学合成および生物学的評価を通じて、高酸素化トロポノイドがPfK1(クロロキン耐性)原虫に対してin vitroで有望な抗マラリア活性を示すことを同定した(図1)。 天然物であるプベルル酸(1),4,5)ビチコリンA(2)およびB(3)6)がin vitroで抗マラリア作用を示すという最初の発見7)により、我々はこのクラスの化合物の構造活性相関(SAR)研究を進めることになった。 (1)の全合成と合成経路を利用した誘導体化により、SARの予備的な結果が明らかになった9)。1のC4位のカルボン酸部分は変換可能であり、芳香環上の3つのヒドロキシ基を含む4つの連続した酸素原子はそのままの方がよい可能性が示唆された。 これまで明らかにされてきた毒性の問題を克服し、経口投与(p.o.)による有効性を向上させるために、我々はC4位を誘導体化し、より詳細なSAR情報を提供することを目指した。 本稿では、C4にカルボニル基を有する新規誘導体の合成とin vitroおよびin vivoでの生物学的評価について報告し、初めて経口活性を有する抗マラリアトロポノイドを発見した。
エステルおよびアミド誘導体のin vitroおよびin vivo抗マラリア評価
合成したエステルおよびアミド誘導体の抗マラリア性を、マラリア原虫PfK1株に対するin vitroおよびヒト二倍体胚細胞株(MRC-5)に対する細胞毒性で評価した13) (Table 1)。 これらの誘導体(6aを除く)は、in vitroでは1と同様に良好な抗マラリア活性を示したが、好ましくない細胞毒性も示した。 また、P. berghei感染モデルマウスを用い、腹腔内投与(i.p.)または経口投与(p.o.)による4日間抑制試験(投与量15 mg/kg × 4)をin vivoで実施した14)。 これらの評価により、i-Prエステル6cおよびt-Buエステル10は、毒性を伴うことなく99%の阻害(i.p.)を示した。 比較すると、他のエステル(6bおよび6d)およびアミド(12aおよび12b)は、中程度の阻害および致死毒性を示した。 驚くべきことに、6cは経口投与(p.o.)でも64%の阻害を示し、毒性はなかった。これは、トロポノイドが経口投与で抗マラリア活性を示すという初めての報告である。 エステルを構造的性質で比較すると、嵩高いエステル6cと10(第二級または第三級アルコールからなる)は、6aと6b(第一級アルコールから合成された)よりも有効である。 これらの結果から、これらのトロポノイドの生体内における抗マラリア活性は、加水分解の可能性に影響されるのではないかと考えられた。 エステル誘導体の強力な抗マラリア特性から、我々はさらなるSARを検討するためにbulky エステルに注目し、6cよりも強力な化合物を作製し、p.o.投与で使用することを目指した。
Table 1.
6dは、c) 。60%の致死率。死因の記載はなし。
n.d.: no data, a) Chloroquine-resistant P. falciparum strain, b) Human diploid embryonic cell line, c) Quit administration after 3 doses due to weight loss, and 3/5 of mice died by day 5.
引用文献
1) “World Malaria Report 2020,” WHO, Geneva, 2020.
2) “Antimalarial drug combination therapy 2001,” WHO, Geneva, 2001.
3) Burrows J. N., Duparc S., Gutteridge E. N., Hooft van Huijsduijnen R., Kaszubska W., Macintyre F., Mazzuri A., Möhre J. J., Wells T. N. C., Malar. J., 16, 26 (2017).
4) Birkinshaw J. H., Raistrick H., Biochem. J., 26, 441–453 (1932).
5) Birkinshaw J. H., Chambers A. R., Raistrick H., Biochem. J., 36, 242–251 (1942).
6) Iwatsuki M., Takada S., Mori M., Ishiyama A., Namatame M., Nishihara-Tsukashima A., Nonaka K., Masuma R., Otoguro K., Shiomi K., Ōmura S., J. Antibiot., 64, 183–188 (2011).
7) Ishiyama A., Iwatsuki M., Yamamoto T., Miura H., Ōmura S., Otoguro K., J. Antibiot., 67, 545–547 (2014).
8) Sennari G., Hirose T., Iwatsuki M., Ōmura S., Sunazuka T., Chem. Commun., 50, 8715–8718 (2014).
9) Sennari G., Saito R., Hirose T., Iwatsuki M., Ishiyama A., Hokari R., Otoguro K., Ōmura S., Sunazuka T., Sci. Rep., 7, 7259–7267 (2017).
10) Mathias L. J., J. Synthesis, 1979, 561–576 (1979).
11) Sawa H., The Chemical Times, 2, 1–7 (2014).
12) Zheng Q., Liu C. F., Chen J., Rao G. W., Adv. Synth. Catal., 362, 1406–1446 (2020).
13) Otoguro K., Ui H., Ishiyama A., Arai N., Kobayashi M., Takahashi Y., Masuma R., Shiomi K., Yamada H., Ōmura S., J. Antibiot., 54, 658–663 (2001).
14) Peters W., Portus J. H., Robinson B. L., Ann. Trop. Med. Parasitol., 69, 155–171 (1975).
15) Lee J. H., Kishi Y., J. Am. Chem. Soc., 138, 7178–7186 (2016).
追加情報 2024/4/7
なぜ紅麹サプリで健康被害が起きたのか…カビ毒の専門家が「プベルル酸とは断言できない」と慎重になる理由
今回は、「プベルル酸の性質」「どのような経路でサプリメントに混入したと考えられるのか」「こうしたカビが作る物質のなにが怖いのか」「ほかの食品にもこうしたカビ毒(マイコトキシン)が含まれるのか」など数々の疑問を、日本のカビ毒研究の第一人者である小西良子・東京農業大学応用生物科学部教授にぶつけました。
https://news.yahoo.co.jp/articles/c76393da6dcc071204722c42cb994f60b893e663
http://blog.with2.net/link.php/36571(ブログランキングをよろしく)